“First comes love, then comes marriage, then comes the baby in the baby carriage!”
This simple rhyme I sang as a child made life, love, and motherhood seem as certain as the rising and setting sun. I carried this idea into adulthood, and was grossly underprepared for the fertility journey my husband and I faced.
My Journey to Motherhood
We tried for about a year before seeking help, and thankfully I got pregnant with the help of hormonal treatments. Due to my short cervix (unknown to me until his 18 week anatomy scan), my son Xavier was born at 21 weeks gestation and died within 10 minutes of being placed on my chest. I spent the greater part of the following year in a fog of grief, followed by a season of healing and restorative rest.
Fourteen months after having Xavi my husband and I decided to try again. In November 2017, I conceived again, this time with a different hormonal regimen. We marked off each week of the pregnancy and I felt more and more optimistic that this time we would get to bring our baby home. To address my cervix issue, I had a cerclage stitch placed at around 12 weeks gestation. Then at 16 weeks I started getting a weekly injection of progestin to help lower the risk of preterm birth. I felt confident that our different approach would have to yield a different result.
Getting to Viability: Ezra’s Birthday
At around 22 weeks my water broke at home and my husband and I rushed to the hospital. Intense waves of anger, grief, and déjà vu flooded me. I was admitted to UAB, and placed on strict bed rest for the first week. In the second week I was moved to the high-risk floor and monitored with fewer movement restrictions. I could go to the bathroom, be wheeled outside, and sit up with visitors. Doctors stood at my bedside daily, reminding me how critical each day in utero was for our baby. Our first goal was to make it to 24 weeks, the age of viability. This number would be the game changer: it meant that life saving measures would be used. Measures that weren’t available for Xavier.
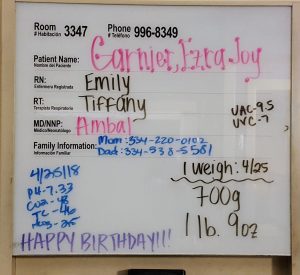
As if she was aware of the time and day, Ezra Joy joined our family in the early morning hours of April 25 at 24 weeks and three days gestation. Like her brother, born alive. Like her brother, less than two pounds. But whereas Xavier and I got to have immediate skin-to-skin time, Ezra was whisked away with a team of neonatologists who had been huddled in the corner during my labor. As the nurse helped clean me up, I received a text message from my dad who had followed my husband and Ezra to the Neonatal Intensive Care Unit (NICU). It was a grainy picture of a tiny red face, with a tiny white hat, wrapped in plastic. My daughter.
The First 24 Hours
Within those first blurry hours of the morning, I demanded a breast pump, as pumping milk was one of the only things I felt I could do in that moment. Nursing staff observed me in recovery for a few hours before I was permitted to see my baby. Before I was permitted. Almost as if she wasn’t even mine.
Once I was cleared, my husband wheeled me into an elevator and took me to the NICU floor. I clenched two one-ounce plastic bottles in my fists with the tiniest amount of thick, sticky colostrum clinging to the sides. Liquid gold the nurses would call it. Words fall short in describing how proud and empowered I felt as the nurse showed me how to dip a cotton swab in the bottle and gently place it on my daughter’s eager tongue.

Life as a NICU Mama
For the next 115 days UAB became our second home. Grateful to live 15 minutes away, we were able to come and go as we pleased or stay overnight as we wished. Those months spent mothering in the NICU forged in me a fierce mama heart. I asked questions — a LOT of them. I kept rigorous notes, with time, dates and the names of anyone who came in to speak with us: neonatologists, respiratory therapists, occupational and speech therapists, nursing staff, residents. I learned to unabashedly advocate for myself and for Ezra. If I had an issue with something, I learned quickly who to speak to in order to see results. I pumped like a cow around the clock and brought so much milk each day that they ran out of room to store it in the NICU freezer. (We were sent home with hundreds of ounces and had to buy a deep freezer, along with storing bottles at friends’ homes!)
We had been told to expect Ezra’s hospital stay to extend at least to her due date, which wasn’t until August. The idea was daunting. Day after day leaving her became more difficult. After praying over her and saying good night, we would drive home and I would ache to be near her again. Many nights and early mornings when I couldn’t sleep for thinking about her, I’d call the NICU and speak with the nurse on call about her vitals, her breathing, her feeds and her output. Anything to stay informed, to feel like she was my child, and not a science project we visited daily.
Ups and Downs of NICU Life
For the most part things went as predicted, but the growth and development of a prematurely born child is in no way linear. Ezra was intubated and extubated multiple times; she would seem to be able to handle lower oxygen settings and then would tucker out and need more assistance breathing. Each day she would progress, and then a few days later have a setback: improvement and regression. This ebb and flow strained my hope until all that remained was a thread. I began to wonder if we’d ever bring her home.

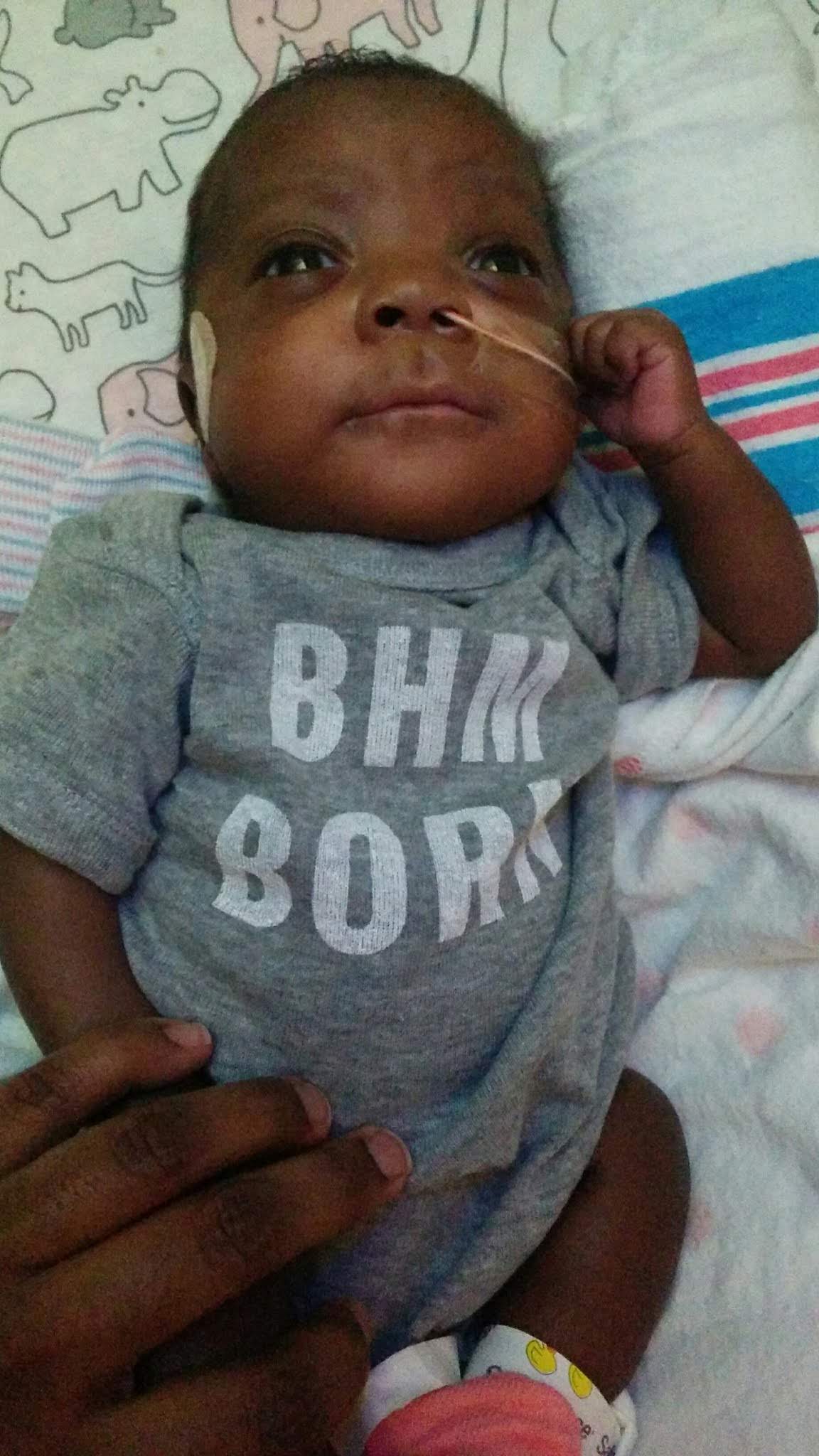
Over time the beeping, dinging, BRADY warnings, and alarms became background noise for me as I sang over her isolette each day. This became our liturgy — slide open room door, set down bag, check vitals on screen, remove jewelry, wash hands up to my elbows for three minutes, dry hands, squirt foam sanitizer in hands, flap hands to dry, open port holes and gently cradle my sweet girl, careful not to overstimulate her delicate skin. I learned from Nurse Paula what was within my rights to ask for — daily skin to skin being one of them.

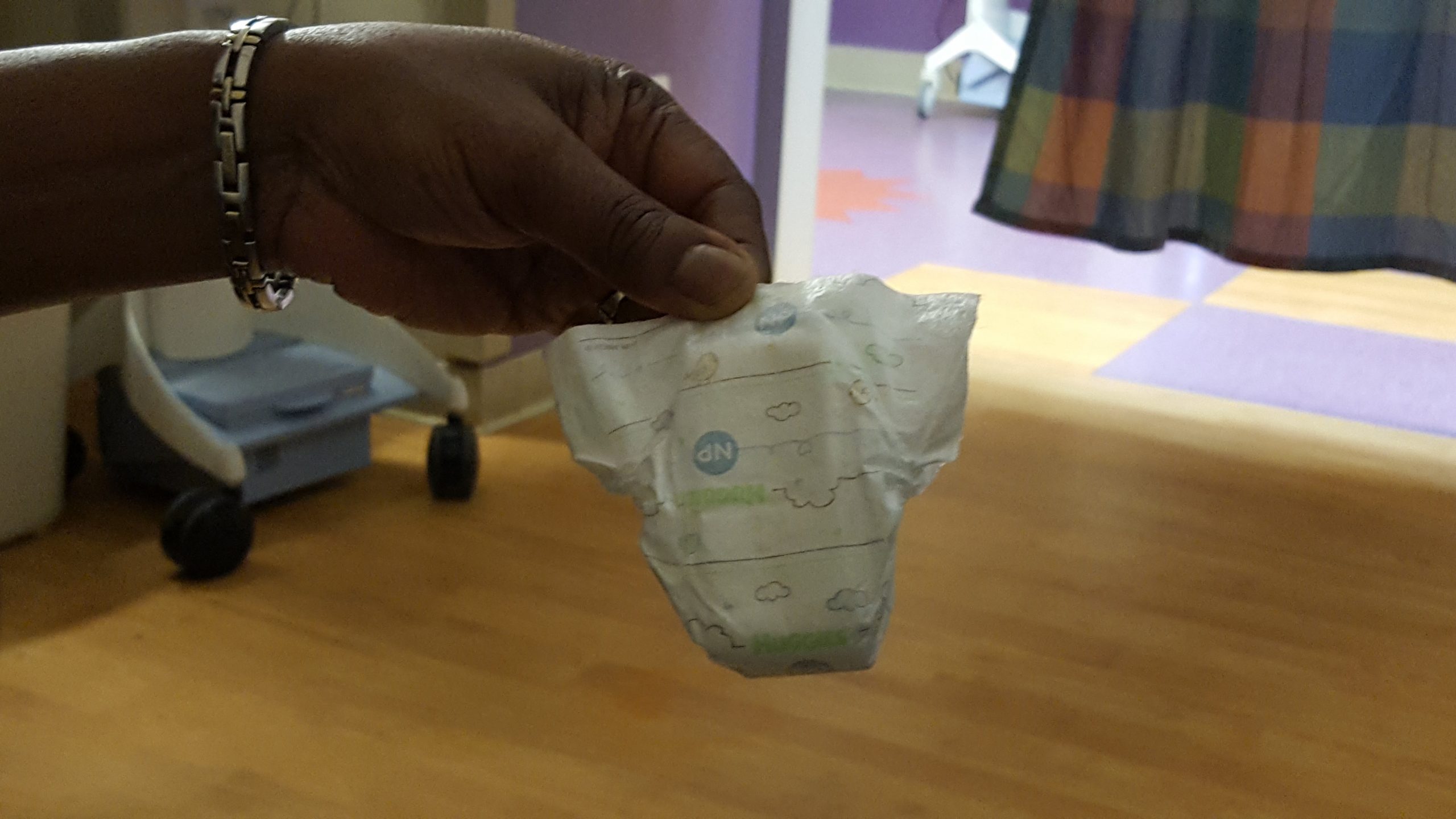
Each day as they placed her tiny body against mine her heart rate steadied, my anxiety washed away, and for those moments we became one. With every shift change, nurses helped ease me into mothering, showing me best methods for changing a micro preemie diaper, teaching me how to pace feed once we started bottle-feeding, and getting up close and personal as we worked on getting her to latch while nursing. I know I was a better-prepared mother because of them.
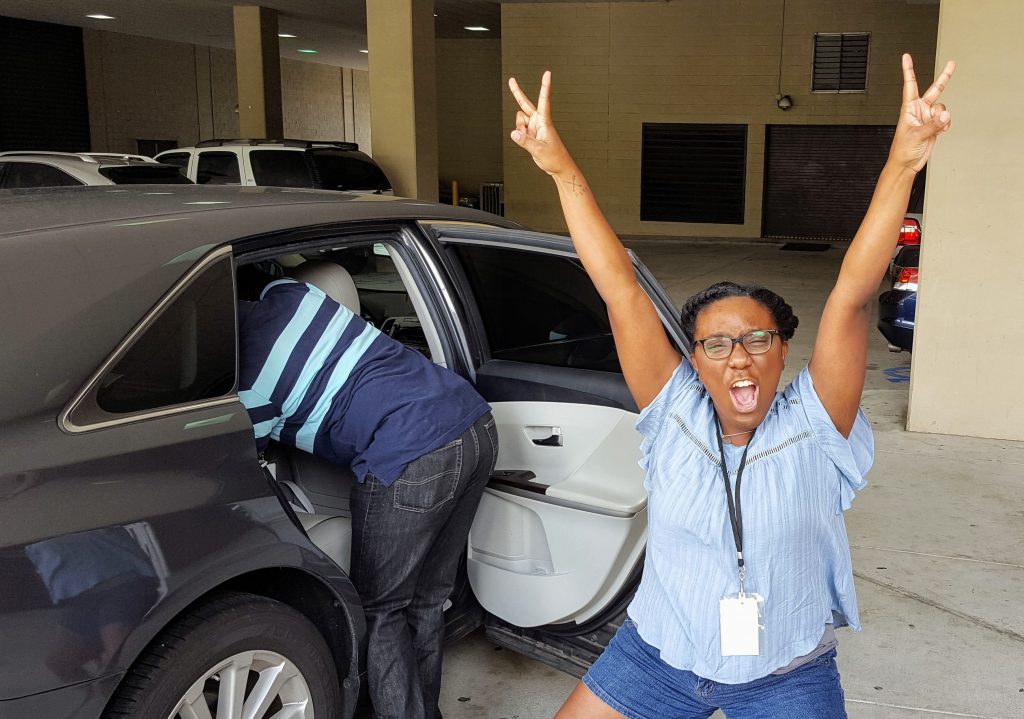
After weeks and months of driving to and from UAB at all times of the day, we finally made it to August. We were still working on getting her to finish all her feeds orally, and we buckled down for two weeks, basically living at the hospital for as long as we could stand. Finally, a week after my original due date we were discharged and brought our sweet girl home.

For the Littles That Don’t Come Home
I am all too aware of the families who don’t have a story that ends like ours. If that is you, Mama, my heart breaks for you. I want you to know you are not forgotten, and I remember you. I remember the baby who roomed next to Ezzi, whose family sat solemnly in the dark amidst the glow of the bili lights. I remember when the dry-erase board of his vitals was cleared and his room emptied to await another family. I remember those whose babies fought like warriors to stay alive, but then took a turn and died in their arms.
I remember the babies who would cry through the night, no family or guardian to comfort them. I learned of the frequency of NICU boarder babies, babies ready for discharge, but with no one to go home to. As one nurse mentioned, the NICU can be a place of parents’ highest highs and lowest of lows. Whether you brought your precious one home in your arms or you carry them in your heart, you are a NICU mama.
Raising Awareness
Organizations like the March of Dimes offer loads of education and resources for families with a child in the NICU. A few other moms have given great insight into how to love on NICU families, and practical tips on navigating the rollercoaster of emotions as a parent of a critically ill child. With September being NICU Awareness month, I would encourage us all to hold space for all the nurses, doctors, and staff that work tirelessly for these vulnerable and precious little lives. I cannot imagine the strain they are facing in light of the COVID-19 health crisis, on top of the everyday challenges that come with their line of work.
Also, I ask that you choose to remember the families: the mothers, fathers, grandparents, aunts, uncles, and friends. They are living in an unprecedented moment, caring for children in ways that they never could have prepared for.
Visit nicuawareness.org for more information on NICU Awareness.